Doc, how did I get this way?
This is a very common question that is brought up during a patient’s initial report. Sometimes seeing the state of their spines can be a shock if they have never seen them before. This is most true for those that “just now” started feeling pain and are dismayed at seeing their spines in such a state of degeneration.
Why don’t we feel the pain until we get into such a state of degeneration or with serious structural issues on the spine that appear to be the cause of such pain cascades? First, understanding how our brain interprets pain and then, second, how did our spines get that way are two areas we need to dive into to answer this question.
How does the brain make sense of pain signals?
Pain messages travel along with the peripheral nervous system until they reach the spinal cord. The gate control theory proposes that there are “gates” on the bundle of nerve fibers in the spinal cord between the peripheral nerves and the brain. These spinal nerve gates control the flow of pain messages from the peripheral nerves to the brain.
Many factors determine how the spinal nerve gates will manage the pain signal. These factors include the intensity of the pain message, competition from other incoming nerve messages (such as touch, vibration, heat, etc.), and signals from the brain telling the spinal cord to increase or decrease the priority of the pain signal. Depending on how the gate processes the signal, the message can be handled in any of the following ways:
- Allowed to pass directly to the brain
- Altered prior to being forwarded to the brain (for instance, influenced by expectations)
- Prevented from reaching the brain (for instance, by hypnosis-induced anesthesia)
The complexity of this process is illustrated by the “phantom limb” phenomenon described earlier in this article, in which pain signals can seem to arise from amputated limbs. The gate control theory provides a framework to explain this by the complex interaction of the structures of the nervous system – and the role of the most complex structure known.
The brain
Once a pain signal reaches the brain, several things can happen. Certain parts of the brain stem (which connects the brain to the spinal cord) can inhibit or muffle incoming pain signals by the production of endorphins, which are morphine-like substances that occur naturally in the human body. Stress, excitement, and vigorous exercise are among the factors that may stimulate the production of endorphins. The impact of endorphins is why athletes may not notice the pain of a fairly serious injury until the “big” game is over. It is also why regular low-impact aerobic exercise.
The brain commonly blocks out sensations that it knows are not dangerous, such as when the feel of tight-fitting shoes that are put on in the morning has all but vanished by the second cup of coffee. A similar process is at work in processing some moderately painful experiences.
The following outlines two briefcase examples of how the gate control theory of pain may be experienced. This case example shows how the experience of pain may change as information is processed in the brain.
- Applying a clothespin to one’s arm initially produces pain that may be quite intense as the skin and surface muscles are compressed. Peripheral nerve fibers detect this pressure and transmit a pain signal to the spinal cord and onto the brain. At first, it is the fast pain signals that get through, and the intensity of the pain experience is fairly proportional to the amount of pressure applied. Everyone would agree that this is acute pain.
- The slower pain signals are not far behind, however, and a dull ache may soon be noticed. After a short while, the pain coming from the pinched tissue will begin to be decreased by the closing of the spinal nerve gates. This is because the brain begins to view the pain signals as non-harmful. The pressure may be painful initially, but it is not injuring the person in any way. As time goes on, the pain message is given less priority by the brain and the person’s awareness of it decreases greatly.
- The brain knows that the clothespin is not causing any injury. Therefore, the brain gradually “turns the volume down” on the pain message to the point of it being barely noticeable after about thirty minutes. The compression on skin and muscle is still occurring, but it is now perceived as a mild discomfort if it is noticed at all.
So, essentially, we may have an acute injury, but we keep on going with our busy schedules, and our brain blocks out the pain—therefore it’s no longer a problem. This sets the stage for chronic compensation which can show up as the occasional “throwing your back out”, or “crick in the neck”.
What we continually see is that the body has been whispering to you for a long time, possibly decades and now the pain or problem is not going away like it used to. It’s sticking around longer, causing more distress, and can make just normal activities of daily living difficult. This is because eventually, as amazing as the human body is, it can no longer compensate for the inflammatory condition that started this snowball in the first place.
The proverbial straw that broke the camel’s back
You see, once our bodies can no longer compensate for the inflammatory condition, it may take simply just bending down to pick up a pencil, turning over in bed, or getting in and out of your car that sparks the “final straw”. The incident will leave you bewildered that it’s all it took, and you may just say, “well, it sucks to get old”, and think that it’s normal—well, IT ISN’T!
Years of chronic compensation of poor posture, sitting too much, sports injuries, slips, falls and auto accidents have left your spine in a condition that has destroyed the proper structure and function of the spinal column. I typically tell patients that it’s never just one thing, but a lifetime of damage that is finally letting you know that it needs help…however we tend to keep going because who has the time for this! I get it! However, how many times has your car broken down and you say the same thing, but you DO take care of it? Why do we take better care of inanimate objects than we do our own bodies? Yes, I’m guilty as well—what do they say, “Doctor heal thyself”? Yeah, I have my moments too, but I also quickly realize the consequences of not listening to my body, I’m reminded every day when I see patient films and hear their histories. It’s being human and living in the fast-paced first world. We blow and go until we can’t anymore and are forced to act—pain is a great motivator, isn’t it?
Let talk degeneration
How does spinal degeneration happen? Let’s look at this from the perspective of an analogy that we can all relate to—what happens to your car tires if you drive with your tires out of alignment?
Right! You get a bald spot on one of your tires and even your brake pads will wear out more on one side. This is how spinal degeneration happens too—when our spine is out of alignment the body tries to stabilize the area by laying down extra bone tissue, resulting in spinal decay and arthritis. This process takes years and possibly decades to occur BEFORE you start to feel the pain that you can no longer ignore and by then permanent damage has already occurred.
Now, let’s look at it from the scientific point of view, for all the nerds out there!
Wolff’s Law
So, why do these changes take place? It’s based on a law of physics called Wolff’s Law. In 1892, Dr. Wolff’s theory about bone transformation was published. One hundred years later, bone remodeling is now a medical fact!
Wolff’s Law states that bone will adapt to the load or stress placed upon it. This means that increased loading of bone tissue will promote increased density. Therefore, many individuals with osteopenia or osteoporosis utilize resistance training to stimulate bone growth. However, when the stress or load on the bone is abnormally loaded, Wolff’s Law can contribute to the progression of spinal degeneration.
A common misconception about spinal degeneration is that it is a normal age-related process. This would mean that most people would exhibit the same level of degeneration at roughly the same age. The truth is that spinal degeneration progresses with time but is not necessarily a normal aging process. There are other factors influencing the progression of spinal degeneration.
In the spine, a similar process plays out with spinal degeneration. As abnormal pressure builds up on the segments of the spine, the increased demand requires more support. The wear and tear associated with increased stress around the joints of the spine will stimulate bone cells to produce hardened tissue to help support the abnormal load. This makes the spine more rigid, and spinal degeneration begins to advance.
How does this process start in the average person? Typically, there is a physical trauma that starts the process. This may be a whiplash injury, car accidents, poor posture, or a jarring force to the neck and spine. This jarring force will cause the alignment of the spine to be compromised. Without proper alignment, the spine cannot move properly, and abnormal stress begins to build. These are very common occurrences, so it makes spinal degeneration a very common finding as we age, but IT’S NOT NORMAL.
Without this normal lordosis (proper spinal curve in the neck), most often the balance of the weight of the head is tilted forward and thus creates increased wear and tear on the intervertebral discs and the vertebral bodies. This eventually leads to bony spurs and osteophytes. Such changes also lead to decreased mobility of the cervical spine and to cervical pain.” From Springfield, Missouri’s very own pain expert, Dr. Norman Shealy (MD / Ph.D.) from an article he wrote for Practical Pain Management back in April of 2009 (Restoration of Normal Cervical Curves).
What are the symptoms of spinal degeneration?
Spinal degeneration develops very slowly over a period of many years. Unfortunately, in the early stages of spinal degeneration, symptoms are very mild and infrequent, which means that many individuals are developing spinal degeneration without any clear indication that their spine is degenerating.
The symptoms of degeneration occur in several stages depending on the severity of its progression. In the early stages, symptoms include:
- Spinal stiffness that improves with activity
- Decreased mobility of the spine
- Intermittent sharp pain
In the more advanced stages of cervical spondylosis, symptoms include:
- Significant decrease in spinal range of motion
- Swelling around the joints of the spine
- Pain that is worse in the morning
- Pinched nerves (numbness/tingling in arms, hands)
- “Grating” sensation when moving the neck or spine
It is important to remember that symptoms alone are a poor indicator of how spinal degeneration is progressing as some may not have any symptoms at all!
“Degenerative changes of the cervical spine are commonly accompanied by a reduction or loss of the segmental or global lordosis and are often considered to be a cause of neck pain. Nonetheless, such changes may also remain clinically silent.” The opening sentences of a study called The Association Between Cervical Spine Curvature and Neck Pain from the May 2007 issue of The European Spine Journal
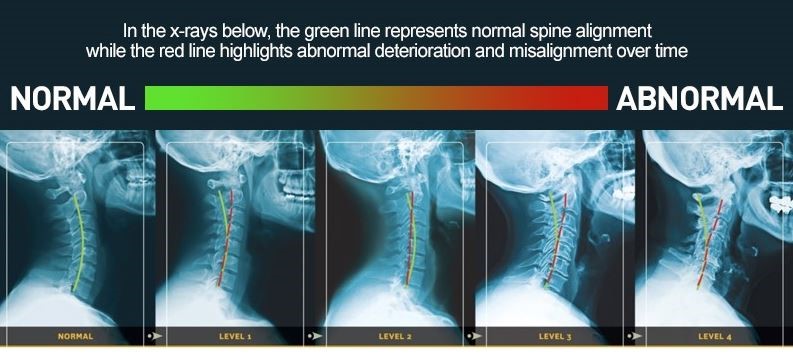
Misalignment over time
I only had a few “minor fender benders”, or “I haven’t had any injuries since High School football”, or my favorite, “it was just a minor concussion” –nothing else that would cause this kind of damage!
Yup, we hear this all the time too. You see, this type of damage takes time to occur—it simply doesn’t happen overnight and, newsflash, healing won’t be overnight as well. But, at HealthWorks Family Chiropractic, we are committed to being your CORRECTIVE CARE CHIROPRACTOR. This means not only will we determine why you are in such pain, but how we can either stop or slow down this degenerative process or hopefully prevent it from happening in the first place. After all, PREVENTION IS THE BEST COURSE OF ACTION!
Our promise to you
HealthWorks Family Chiropractic is dedicated to a comprehensive and specific approach to taking care of spinal and nervous system needs. Let us help you find out how taking care of the most important system in the body will create optimal health that will last a lifetime! Remember, I’ve been where you have been. I have seen and felt the difference gentle, corrective, upper cervical specific chiropractic care has made in my life. I really hope the same for you and your family. Act and beat the causes of spinal degeneration and pain today!
- Dr. Norman Shealy, MD, Ph.D. Practical Pain Management April 2009: Restoration of Normal Cervical Curves.
- Grob D, Frauenfelder H, Mannion AF. The association between cervical spine curvature and neck pain. Eur Spine J. 2007;16(5):669-678. doi:10.1007/s00586-006-0254-1